Story and photos by Jessica Campbell
Reporting by Jessica Campbell and Allylah Msenya
ELDORET, KENYA — At the Moi University Teaching and Referral Hospital (MTRH), it is not uncommon to see the same patient more than once. But what if it is not sickness causing the patient to return to the waiting room once a week? What if it is because the drugs given do not actually contain medication?

The supplies needed to run a Paper Analytical Device for counterfeit drugs.
In a 2005 survey conducted by National Quality Control Laboratories, 30 percent of all drugs distributed to the public were counterfeit. Counterfeit drugs are a huge problem.
But now a device called the Paper Analytical Device (PAD) is being piloted in Kenya by the pharmacists employed at the MTRH.
The device provides an easier, faster and far less expensive way to assess the drug’s authenticity, and provides a more sustainable schedule for taking and keeping track of one’s medication.
The main method for testing counterfeit drugs is to use a high performance machine. It’s a technology that cannot be found in Kenyan hospitals.Because it cost nearly $500 to test a batch of drugs with this method, there was virtually no way to determine if an imported pharmaceutical was genuine. A cheaper screening system has been sorely needed.
The PAD, designed and manufactured at the University of Notre Dame in Indiana, is a small, easily transported paper-based device that costs about 40 cents to manufacture in the U.S. Testing with the PAD is done on an individual basis, with one drug at a time.
The tester takes a pill and scrapes it horizontally across the paper, leaving the pill’s residue. The PAD is then placed in a small cup of water, which ignites a reaction between the water and chemicals constructed within the pad. The water rises slowly, producing various colored lines. Each color represents a substance inside the pill.
Currently, the PADs are only being used to test a few specific drugs, such as Amoxycillin, Ampicillin and Acetaminophen. There is also a separate PAD designed to screen tuberculosis drugs.
As of now, the PAD is being made in Indiana and shipped to Kenya. At the MTRH, pharmacists on the project are collecting samples of the drugs, testing them, and then taking photographs to send back to Notre Dame for validation.
One of the managers working on the PAD project in Kenya, Mercy Maina, views the device as progress for the health and well being of many patients throughout the world.
“When you see someone [a patient] after giving them medication and they do not improve and you find out it might actually be the medication, it is very frustrating,” Maina said. “We are hoping to change that with this project.”
Maina describes the project in two parts, optimization and validation.
“The optimization is just talking about making it [PAD] better in terms of the format, its sustainability and testing that out,” she said. “After we optimize the test we hope to validate it because there is no way to guarantee the results yet.”
According to Maina counterfeiters increasingly dilute the amount of active ingredient in the drug by adding fillers.
“Counterfeiters are evolving with us,” she said.

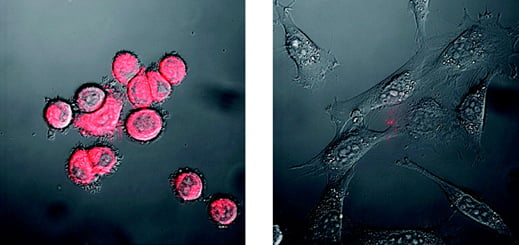
The resulting Paper Analytical Device after running a counterfeit test on an antibiotic drug.
If the drug has been tampered with, the colors that are supposed to appear when tested show incorrect intensities.
Unfortunately, the PAD only tests the quality of a counterfeit drug, not the quantity of fake substances, so the degree to which counterfeiters have tampered with the pills cannot be determined by those testing the drug.
“It is not less accurate, it just won’t tell you the exact amount of the foreign substance,” Maina said. “That is why we are promoting it as a screening device now.”
Ashley Scott, a master’s student in global health, worked on the PAD project while a Notre Dame. She is currently in Kenya teaching other pharmacists and students how to conduct and accurately read the tests.
“What is great about them [the tests] is that you do not need any pharmaceutical expertise,” she said. “It takes about an hour for others to learn how to use the PAD.”
But with so many people testing, the interpretations of the PAD results can be diverse. Removal of the bias is the next step in making the device more stable. In the future, the tester will take a photo with a cell phone and send it to a link established on a universal website. Then computer software will analyze the test and send back the result. The software will also confirm any results deemed positive or negative that may have falsely been identified.
Maina said the tests work fairly well, with less than 10 percent of them giving false indications.
Sonak Pastakia, a pharmacist working with AMPATH, brought the idea from Notre Dame to Kenya. AMPATH is the Academic Model Providing Access to Healthcare, a consortium of ten North American universities lead by Indiana University in partnership with Moi University and the MTRH.
“I loved the idea and thought it could dramatically improve the situation with regards to counterfeit medication detection,” he said, “Ever since I set foot in Kenya and realized how incredibly difficult it is to treat patients when you can’t trust the products you are giving them, I have wanted to convert the technology to Kenya.”
Patients can lose trust in their doctors when they are given drugs but do not get well. according to Maina.
“You can die, there are people who have had serious allergic reactions and it affects the larger public health spectrum,” she said. “Why the hell should a patient trust me as a public healthcare provider if the drugs I am giving them are counterfeit?”
Once the distribution of the PADs expands, which Maina said she hopes is by the end of the 2013 year, the members on the project hope to expand the technology of the paper-based devices to other uses, such as evidence testing.
For those patients on medication, teaching them how to test their own urine may allow them to monitor their condition more accurately.
“You ask people, ‘are you taking your drugs?’ and they say yes, even when they aren’t” Maina said. “So, I can tell you to pee in a cup and I can test for the certain drugs and tell if you are or are not taking the drugs.”
Maina said patient in the future could test themselves at home, then text or send in a sequence of numbers generated by the test that would confirm whether the prescribed drugs are being taken.
“Creating specific pads for specific drugs and diseases, that is where we are going in the future,” Maina said.